I’ve mentioned previously that food for our family can be difficult and I often get asked if Bean can eat. The answer to that is, yes, er…most of the time. It depends. I mean… it varies, and she has a pretty…complicated diet.
Beanie is dependent on total parental nutrition (TPN), meaning that she gets nutrition in an intravenous (IV) form. She is hooked up to an infusion through her Broviac line between 12-18 hours/day and that infusion contains carbohydrates, protein, vitamins and some of the time, fats. When she is doing well, her TPN calories are minimal and she eats/drinks a decent amount. Other times, she gets 100% of her calories in her TPN and eats nothing or very minimal. Every time she gets sick and is in the hospital for awhile, she always seems to end up back on full TPN and doesn’t eat much (if anything) for the first week or so home. If she is doing well and hasn’t been ill, she is likely getting less calories in her TPN. Also, even when she is doing well, she’ll occasionally have a random day or two where her belly is more irritable than usual and we won’t let her eat anything to give her gut some rest. (See, what I mean with that super straightforward answer?)
Her second source of nutrition is from specialty prescription formula called Pediasure Peptide. It is a complete liquid nutrition source (kind of like Boost that you can buy in the grocery store but fancier). It is partially broken down so her weak intestines can absorb it more easily. We call this her “milk.” It’s pretty calorie-dense and she seems to tolerate it well. However, some days she drinks it super well and other days she won’t touch it. (Aren’t toddler/preschooler opinions awesome?) There may come a day when we consider having a feeding tube placed in her stomach so she can take in more of this in hopes we can reduce the calories in her TPN and possibly have periods of time when she doesn’t need TPN at all.
Her third source of calories are FOOD and sister loves to eat. Food with Beanie has been rocky from the start. Her first hospital admission was at 7 months (when she was officially diagnosed with MMIHS), shortly after we introduced solid foods. Since then we have identified a long list of “trigger” foods that exacerbate her condition one way or another. This has been done with some medical & dietician guidance and some through rocky trial and error.
What can’t she eat?
Things like raw vegetables are a hard no-go. They are difficult to break down and tend to “clog” her up. Many cooked vegetables still cause problems, but we have found a few that are OK. With a food processor and an instant pot, I’ve been able to work in things like carrots, zucchini & squash as well as spinach and peppers as long as it is pureed and cooked well. She primarily eats foods that are low-residue, so things without skin and seeds (again, they clog her up). She does OK with some fruits in small amounts with small seeds, like strawberries and kiwi.
The next no-goes are a doozy.
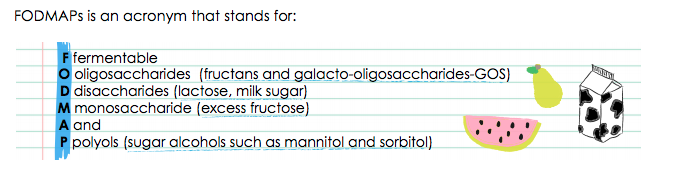
Elli follows a modified Low FODMAP diet. You probably just thought “What the heck is that?” Well, it’s ridiculous, that’s what it is, but it seems to help her and us parents will do almost anything for our kids, so I’ve let this diet take all of us down a completely trying and many-tears-worthy road of trying to find foods that Beanie can eat. FODMAP is an acronym for all things good. Not really, but some days it seems like it. In reality,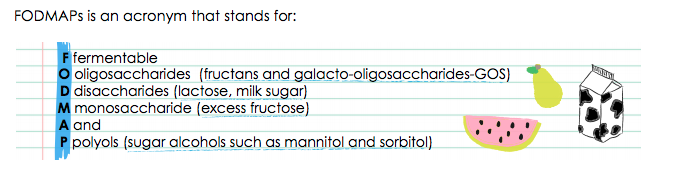 FODMAPS are carbohydrates that are poorly absorbed in the small intestine. They are found in loads of common foods such as wheat, barley, rye, apples, pears, mango, onion, garlic, honey & beans. They contribute to gas production. Since bloating/distention is a huge issue for Beanie (Yes, I know it’s ironic that I call her Bean and she CANT EAT BEANS), we considerably limit the amount of FODMAPS in her diet. If you want to learn more about the diet in detail and would ever want to try your hand at Low FODMAP cooking, check out this blog. (Yes, I ripped the acronym illustration off from the author). Here is a good one-page reference that goes into the science behind the diet a bit. The diet is primarily designed for patients with IBS, but the reasons why it works for those are also many of the same reasons why it seems to limit some of her symptoms that spur from her poor gut motility.
FODMAPS are carbohydrates that are poorly absorbed in the small intestine. They are found in loads of common foods such as wheat, barley, rye, apples, pears, mango, onion, garlic, honey & beans. They contribute to gas production. Since bloating/distention is a huge issue for Beanie (Yes, I know it’s ironic that I call her Bean and she CANT EAT BEANS), we considerably limit the amount of FODMAPS in her diet. If you want to learn more about the diet in detail and would ever want to try your hand at Low FODMAP cooking, check out this blog. (Yes, I ripped the acronym illustration off from the author). Here is a good one-page reference that goes into the science behind the diet a bit. The diet is primarily designed for patients with IBS, but the reasons why it works for those are also many of the same reasons why it seems to limit some of her symptoms that spur from her poor gut motility.
Through trial and error, we have learned that some FODMAPS irritate her more than others, so we don’t follow the diet to a strict rule, but the basics for feeding Beanie include avoid:
- Wheat (Anything with regular flour in it is on the “no” list).
- Onion (These really seem to set her off)
- Beans/Legumes/Lentils (Hello…they make you gassy. Of course they wreck havoc on her)
- Lactose (We do lactose-free dairy products and there are a couple things she does OK with in small portions).
- Soy
- High fructose corn syrup
- Garlic chunks (She does OK with a little bit of garlic powder, but no garlic-press for me anymore!)
- Apples, pears, peaches (we are SLOWLY testing out some fruits)
- Peas (including pea protein and pea flour)
- Broccoli & cauliflower (back to things that make you toot).
- Inulin (this is an additive in a lot of processed “healthier” foods…especially gluten free foods, which is a major bummer because we are avoiding wheat, so I shop a lot in the GF aisle).
- Coconut (not a big deal until you realize that coconut flour is often used in place of wheat flour)
Yep. That’s a stupid list. The first time I met with a dietician about this diet I cried legit tears. For a while I felt like there was NOTHING she could eat. Some days, I still feel like that. We have attended multiple gatherings (Family events, holiday/birthday parties, Church dinners) were literally the only things she could eat where tortilla chips and rice…and sometimes the rice is tainted. I always try to pack something she can have so she doesn’t sit and watch people eat around her. The few times I forgot have really made me feel like an awful parent as I tell Bean that she can’t eat because everything we have will make her tummy upset. This usually results in us both going and crying somewhere there is no food around.
So, what DOES she eat?
- Protein is her friend (All FODMAPS are carbs). We do a lot of eggs, chicken, turkey, fish, beef. Skip the breading (unless you’ve done your homework), garlic & onion and learn about different spices to use.
- Rice-based carb stuff. We buy a lot of “gluten free” pasta, bread, cereal, etc. However…read the stupid label because there is a 50/50 shot inulin or pea flour/coconut flour is hiding in there
- Corn-meal based carbs (cornbread—as long as there is no wheat flour, grits, corn tortillas).
- Potatoes (but fried food makes her yack, so bake the fries, please).
- Lactose-free dairy products. (Fun fact—cheddar is lactose free. Cheese can cause it’s own problem with her, so we don’t let her chow down on cheese, but some cheddar in a soup or casserole is OK).
- Some fruits in moderation such as bananas, cantaloupe, kiwi, peeled grapes (torture!), mandarine oranges.
- Cheerios (and a handful of other wheat-free toddler staple foods). I found a substitute for goldfish crackers recently and felt like I won the lottery.
I’ve became a master label-reader. In this post, I’ve only covered about the top 25% of the whole FODMAP containing food list, so in no way is this inclusive. One of the tricky things is learning which brands of foods are OK. Pantry “staple” foods such as ketchup, chicken broth, tomato sauce, peanut butter & jelly all vary A LOT as far as ingredients go. So, what is OK in one brand may not be in another. If you ever decide you want to cook for Bean and the recipe says to use the Progresso low-sodium Chicken Stock in the soup, that means something, because the regular Progresso Chicken Stock or Progresso Chicken Broth both have onion in them.
Also, portion-size matters. There are a lot of foods that have small amounts of FODMAPS in them, so we can do up to a certain amount. Yes, I have an app for this. It was $8 and worth every penny, and I hate paying for apps.
Oh yeah, we also try to increase, but not overdo, her oral intake of essential fatty acids when she is not getting fats in her TPN. The fat in her TPN, or “Lipids,” come with the highest risk of complications, so we try to avoid using them as much as we can. So, we try to get her to eat the needed amount of fats every day. Pro tip–put margarine on everything of hers that you can. Yes, margarine, not butter, because, again…that matters. (For the food geeks reading this–margarine has a greater concentration of essential fatty acids than butter does…more bang for your buck).
It’s a lot and it took me MONTHS to figure out a lot of the kinks. There have been weeks where the only thing she has ate were scrambled eggs & cheerios (with lactose free milk in both). However, it has gotten easier. I’ve found “safe” cupcakes for birthday parties, modified some of our standard rotating meals to work and joined a couple of super helpful Facebook groups that are moderated by dietitians who can answer questions about recipes and portion sizes. Finding foods for her to eat have been worth it and I would do it all again. Sister loves food and she gets it from her mama. Now, hopefully, you’ll understand a bit more why a dinner or party invitation stresses me out a little more than the average mama bear.
Is your head spinning yet? Can we come over to your house for dinner tomorrow night? I’m tired of cooking. I can give you the recipe with brand-specific shopping list. 😉



 FODMAPS are carbohydrates that are poorly absorbed in the small intestine. They are found in loads of common foods such as wheat, barley, rye, apples, pears, mango, onion, garlic, honey & beans. They contribute to gas production. Since bloating/distention is a huge issue for Beanie (Yes, I know it’s ironic that I call her Bean and she CANT EAT BEANS), we considerably limit the amount of FODMAPS in her diet. If you want to learn more about the diet in detail and would ever want to try your hand at Low FODMAP cooking, check out this
FODMAPS are carbohydrates that are poorly absorbed in the small intestine. They are found in loads of common foods such as wheat, barley, rye, apples, pears, mango, onion, garlic, honey & beans. They contribute to gas production. Since bloating/distention is a huge issue for Beanie (Yes, I know it’s ironic that I call her Bean and she CANT EAT BEANS), we considerably limit the amount of FODMAPS in her diet. If you want to learn more about the diet in detail and would ever want to try your hand at Low FODMAP cooking, check out this 
 One of the worst things about having a kid with a rare disease is how lonely it can be. Knowing no one who can relate or understands what you are going through is an isolating experience. For almost the first two years of Bean’s life, this was the situation or family was in. Up until very recently, she has been the only child seen at her hospital with the disease. We knew there were other families out there, but didn’t know how to find them or where they might be.
One of the worst things about having a kid with a rare disease is how lonely it can be. Knowing no one who can relate or understands what you are going through is an isolating experience. For almost the first two years of Bean’s life, this was the situation or family was in. Up until very recently, she has been the only child seen at her hospital with the disease. We knew there were other families out there, but didn’t know how to find them or where they might be.
 completed a residency and are training to become a specialist). The admission ended with our family being transferred to the care to the Gastroenterology team. The GI physicians have became like sometimes adored, sometimes despised, slightly dysfunctional (yet brilliant), distant family members, who are permanent fixtures in our lives. Nearly the entire GI department gets a Christmas card from us every year—for good reason.
completed a residency and are training to become a specialist). The admission ended with our family being transferred to the care to the Gastroenterology team. The GI physicians have became like sometimes adored, sometimes despised, slightly dysfunctional (yet brilliant), distant family members, who are permanent fixtures in our lives. Nearly the entire GI department gets a Christmas card from us every year—for good reason.